
Itโs harder for Americans to get access to prescription drugs, even with insurance, research shows
Itโs harder for Americans to get access to prescription drugs, even with insurance, research shows
For Americans navigating the pharmacy counter, the price of a prescription is often just the beginning of the story. Behind that cost lies an increasingly complexโand often opaqueโnetwork of coverage decisions that determine which medications are available and under what conditions.
New data from Research reveals just how inadequate and restrictive prescription insurance has become.
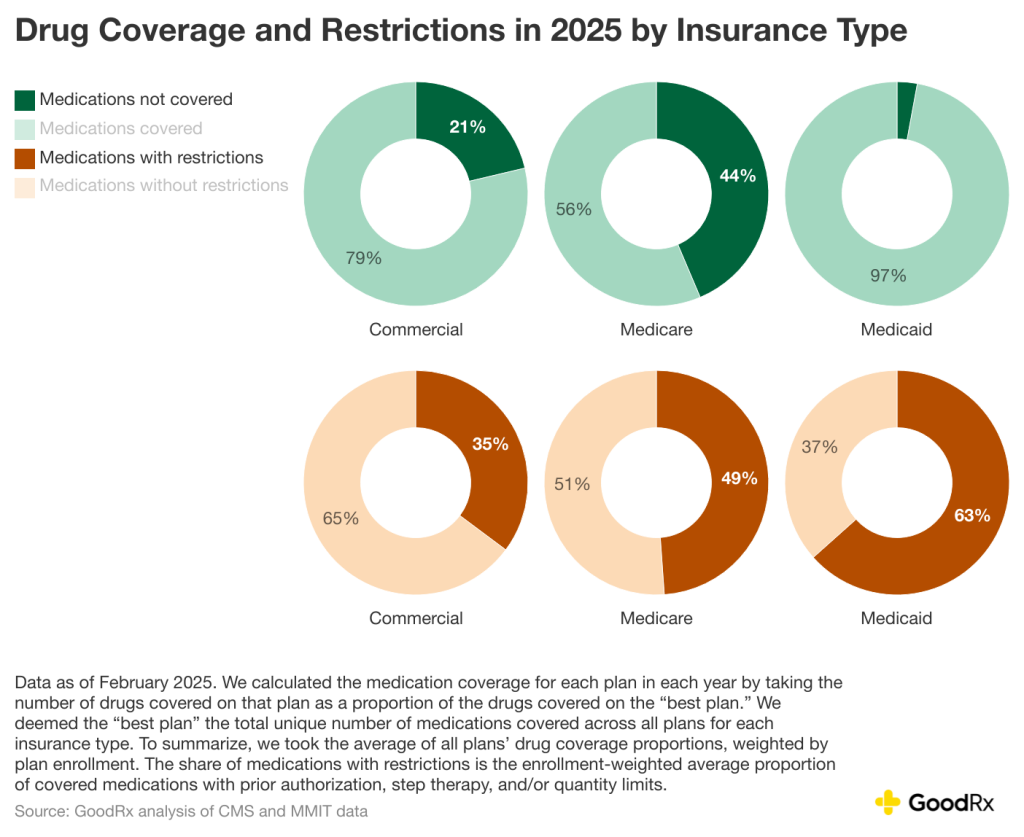
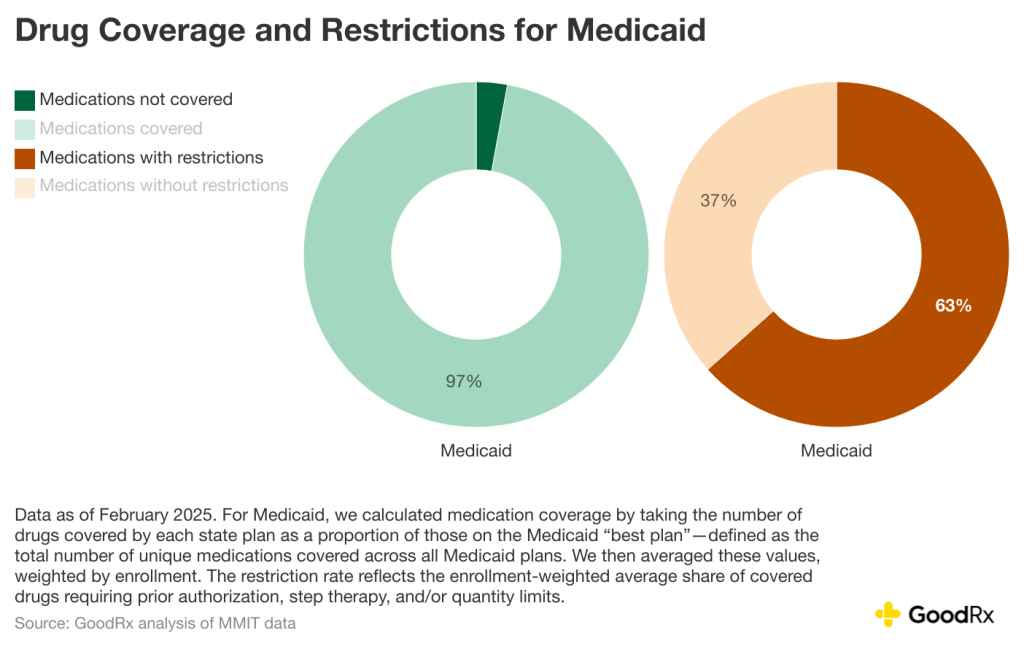
Medicaid, often viewed as a safety net, covers the broadest share of prescribed drugs but imposes more restrictions than any other insurance type. , by contrast, covers the least drugs while restricting access for nearly half of the drugs that are covered. Commercial insurance, typically employer-sponsored or purchased individually, falls in the middle in terms of drug coverage but has the fewest coverage limitations, like , , and .
Key takeaways:
- New data from GoodRx Research shows that prescription insurance coverage is less comprehensive and more restrictive across all insurance types.
- For the average commercial insurance plan, 21% of medications have no coverage and 35% of covered medications have restrictions, like prior authorization.
- Medicare coverage is even worseโthe average Medicare plan doesnโt cover 44% of medications and imposes restrictions on nearly half of the medications that are covered.
- While the average Medicaid plan covers 97% of medications, 63% of those medications require additional steps to obtain coverage, like prior authorization.
The findings offer a stark reminder: For many Americans, the real hurdle to treatment isnโt just medication pricesโitโs navigating the complex policies embedded in their health plan that dictate the cost they pay at the pharmacy counter.
Commercial insurance: Coverage gaps and red tape
Nearly are covered by commercial insurance plans. Many people enroll in these plans through their employer, though they can be purchased on the individual market as well. While commercial plans are the dominant form of coverage in the U.S., they cover just under 80% of prescription medications for the average enrollee. This means that patients may face the full prescription price at the pharmacy counter for 1 in 5 medicationsโeven after paying .
This coverage gap becomes even more troubling when you peer behind the red tape: 35% of the drugs that are covered are subject to restrictions like and step therapy.
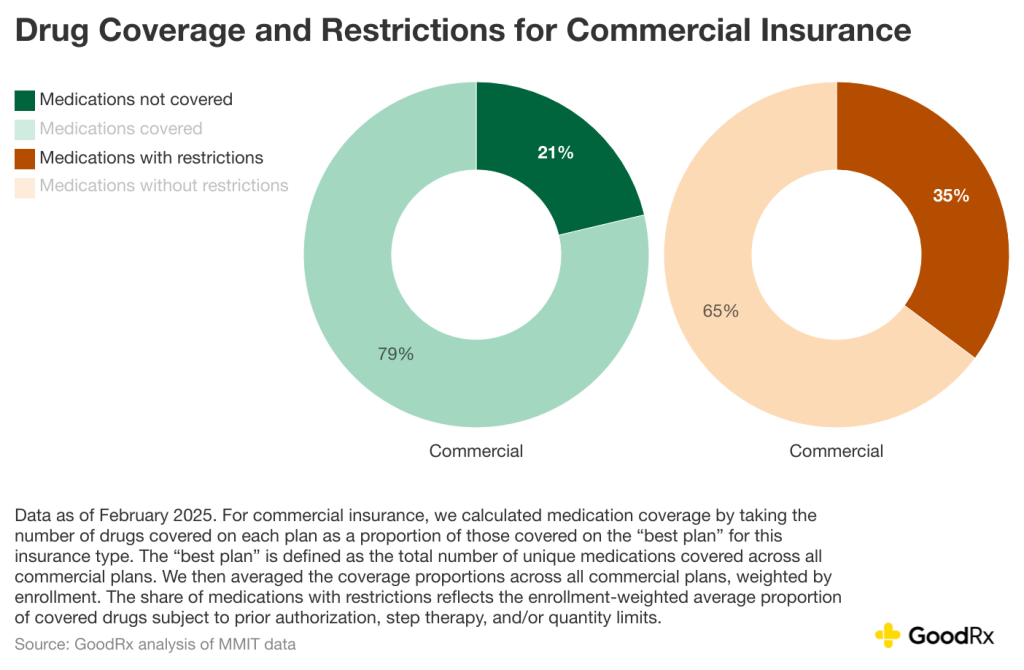
In practice, this means more than a third of drugs listed on a planโs formulary arenโt easily accessible. Patients may be required to try and fail on cheaper alternatives first, or their physician may need to justify the prescription multiple times over.
These requirements can delay care, burden healthcare professionals with paperwork, and ultimately lead patients to abandon treatment altogether. In fact, according to GoodRx Research, over facing insurance restrictions declined to go through the process, opting instead to fill a different medication, pay cash, or . Over half (56%) who did go through the process said the extra steps made them consider stopping their medication altogether.
The reality for many is that coverage doesnโt automatically mean access. As plans tighten formularies and increase utilization management, patients are left navigating a bureaucratic maze in search of relief.
Medicare: Fewer drugs, more barriersโeven in protected classes
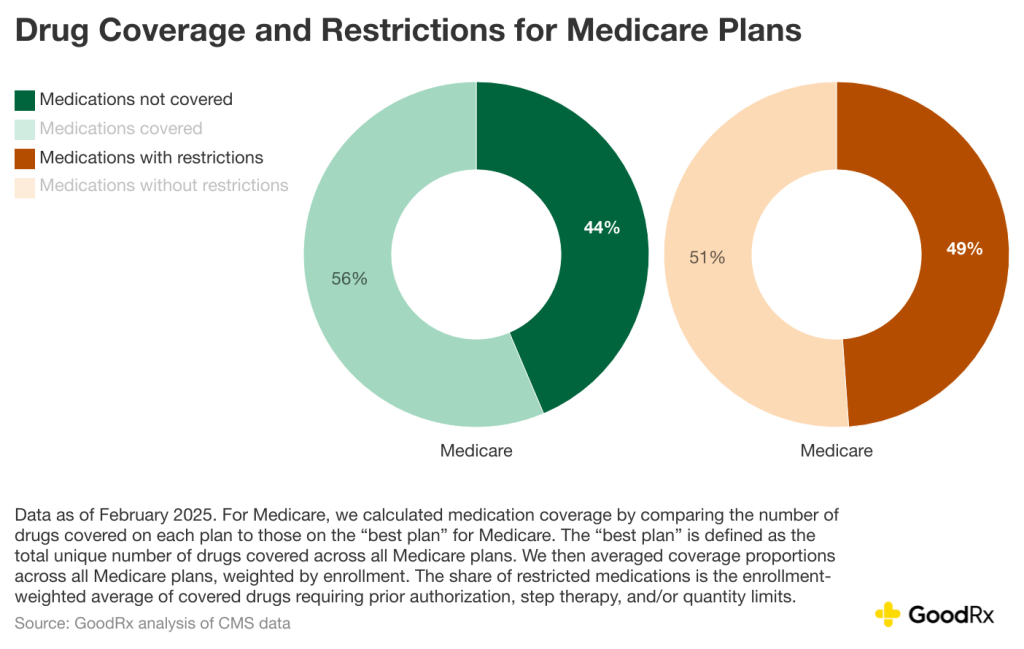
If commercial insurance presents a coverage puzzle, offers its own paradox. Medicare is a critical source of coverage for vulnerable beneficiaries, including older adults and people with disabilities. Nearly are on this plan. Yet, among the three major channels, Medicare plans cover the fewest drugsโjust 56% of those analyzed as of February 2025.
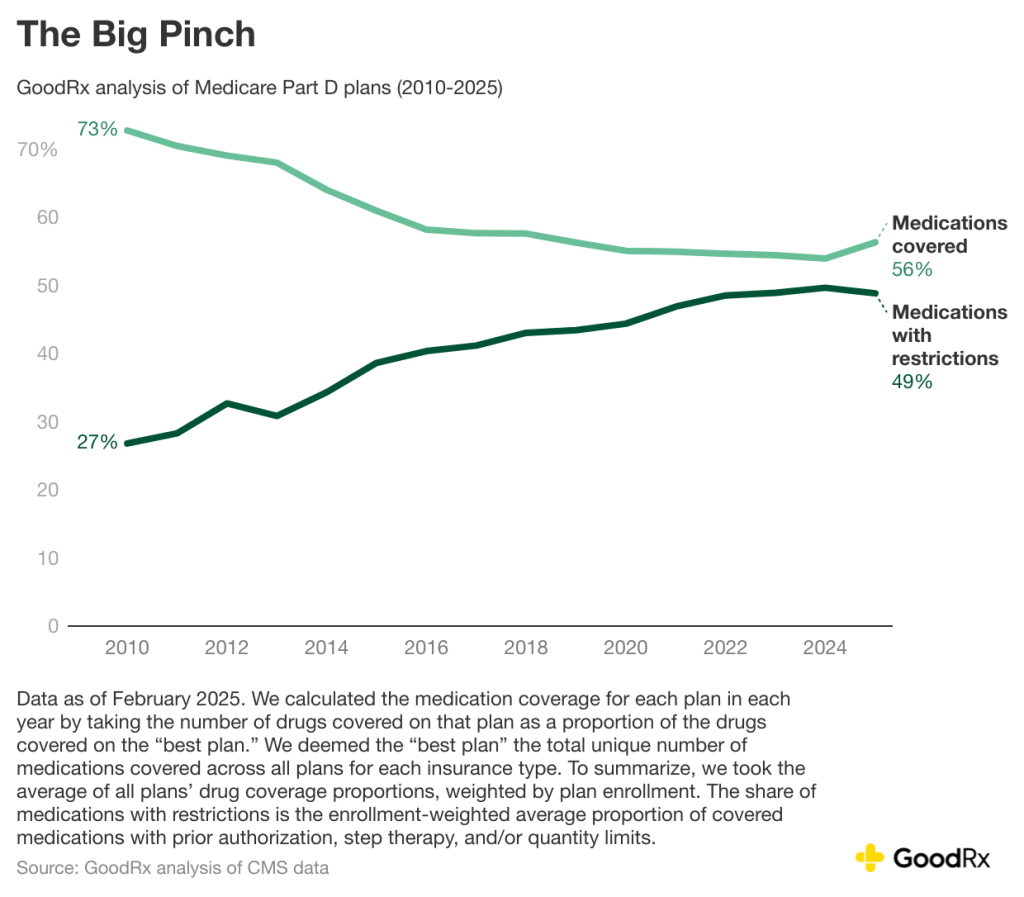
Thatโs a steep drop from the 73% coverage in 2010, according to GoodRx data. But for the first time in years, that downward trend may be leveling off. This yearโs updated figures show a modest uptick in the number of drugs covered by Medicare plans, along with . This is a rare bit of good news in an otherwise tightening system.
Still, the broader story remains complex. To protect vulnerable beneficiaries, Medicare imposes federal requirements on drug plans that aim to guarantee access to critical treatments. Chief among them is the mandate to cover โall or substantially allโ drugs in six protected classes:
- (used after organ transplant)
- (for HIV/AIDS)
- Antineoplastics (for )
These categories were selected because of their clinical importance and the potential harm in the case of limited or interrupted access. Plans must include at least two drugs in all other therapeutic classes, but for these six, theyโre expected to cover nearly every formulation.
But, again, coverage does not guarantee access. And thatโs true even within these federally protected classes.
Nearly half (49%) of the drugs covered by Medicare plans are subject to utilization management tools like prior authorization and . This includes medications in the protected classes themselves.
In practice, this can mean delays, , or complicated for people who need timely care. For instance, a cancer drug may appear on a formulary but still require layers of paperwork before treatment can begin. Or a patient may have to cycle through before gaining access to the one their healthcare professional originally prescribed.
Such restrictions are part of a broader pattern GoodRx Research has identified: Insurance plans are covering fewer medications overall, while placing more conditions on access to those they do cover. Thatโs left many Americans caught in what weโve called the โwhere price is only part of the problem, and the real hurdle becomes navigating increasingly burdensome policies. The pressure is even being felt in Medicare, where federal protections are meant to insulate beneficiaries from the worst of these dynamics.
While the pinch let up some this year, it certainly isnโt gone. The average Medicare beneficiary still lacks any coverage for 44% of medications eligible for Medicare coverage. And that doesnโt include the medications that are explicitly from Medicare coverageโincluding treatments for conditions like obesity and weight loss.
In short, Medicare's safety nets still matterโbut theyโre being stretched. The programโs federal protections offer a vital floor, yet cost-containment efforts and restrictive policies continue to erode the certainty of access that many beneficiaries expect.
Medicaid: The most generous, but not without trade-offs
Medicaid stands out as the most comprehensive of the three insurance sources. The average Medicaid plan covers 97% of drugsโsignificantly higher than both commercial and Medicare plans. However, 63% of those drugs come with restrictions, the highest of any coverage type.
This trade-off affects a substantial share of the countryโ are enrolled in Medicaid. For many, itโs the only source of prescription drug coverage.
That high rate of restriction reflects efforts to control costs in state-run programs operating on limited budgets. But it also points to a tension: Medicaid provides the broadest safety net in terms of whatโs covered, but not necessarily in how easily patients can access that coverage.
For individuals with low income who rely on Medicaid, the abundance of covered drugs may be undercut by administrative burdens. The path to getting medication can still be filled with delays, appeals, and denialsโall of which add friction to an already fragile system.
Methodology
Commercial insurance and Medicaid:
We sourced commercial and Medicaid formulary data from Managed Markets Insight and Technology, LLCโข, a trademark of MMIT. Data reflect coverage as of February 2025 for all drugs present in the formulary since Q4 2024, excluding over-the-counter medications and those administered by healthcare professionals. Commercial insurance plans include employer-sponsored plans and health exchange plans. Medicaid plans include managed and state Medicaid plans.
We calculated the medication coverage for each plan by taking the number of drugs covered on that plan as a proportion of the drugs covered on the โbest plan.โ We deemed the โbest planโ the total unique number of medications covered across all plans for each insurance type. To summarize the data at the channel level, we took the average of all plansโ drug coverage proportions, weighted by plan enrollment.
We calculated the share of medications with restrictions as the enrollment-weighted average proportion of covered medications with prior authorization, step therapy, and/or quantity limits.
Medicare:
We sourced Medicare formulary data from the Prescription Drug Plan Formulary, Pharmacy Network, and Pricing Information files. Data reflect coverage from Q1 2010 through February 2025. Our analysis does not include National PACE plans, employer-sponsored plans, and demonstration plans per Medicareโs documentation.
We calculated the medication coverage for each plan in each year by taking the number of drugs covered on that plan as a proportion of the drugs covered on the โbest plan.โ We deemed the โbest planโ the total unique number of medications covered across all plans for each insurance type. To summarize the data at the channel level, we took the average of all plansโ drug coverage proportions, weighted by plan enrollment.
We calculated the share of medications with restrictions as the enrollment-weighted average proportion of covered medications with prior authorization, step therapy, and/or quantity limits.
Amanda Nguyen and Sasha Guttentag contributed to this article.
was produced by and reviewed and distributed by ย้ถนิญดด.



