
8 statistics that explain the rural doctor shortage
This story originally appeared on Incredible Health and was produced and distributed in partnership with 麻豆原创 Studio.
8 statistics that explain the rural doctor shortage
For Americans who live in cities or suburbs, going to the doctor is usually a simple errand. Even if they have trouble finding an appointment time that works for their schedule or getting their health insurance to cover it, their doctor's office or hospital is usually a manageable distance from their home or work.
However, for , accessing healthcare isn't as easy. According to a 2018 survey by the Pew Research Center, nearly a quarter of rural Americans say for their community. Making things worse, these rural residents tend to be than their urban and suburban counterparts.
The challenges preventing rural Americans from accessing medical care will likely worsen. The Association of American Medical Colleges projects in the United States by 2033. Residents of will see their travel times to doctors and hospitals increase even more.
Of course, not every doctor's visit requires in-person care: Telehealth is becoming more popular, thanks in part to and the during the COVID-19 pandemic in 2020 and 2021. However, many people in rural areas also 鈥攚hich renders telehealth visits nearly impossible.
To understand the effects of the rural doctor shortage in the United States, compiled data from government entities and research institutions. Here's what you need to know about the current lack of medical care in rural communities, the effects the shortage has on patients, and the outlook for health care in rural areas.

Nearly 4 in 5 rural U.S. communities are short on medical staff
According to , 60% of the areas in the United States that are designated as "medically underserved"鈥攎eaning they 鈥攁re rural. Even more troubling, the average age of rural physicians is older, which means . There has also been a decline in the number of , who historically are more likely than their urban- and suburban-raised peers to practice medicine in rural areas as adults.
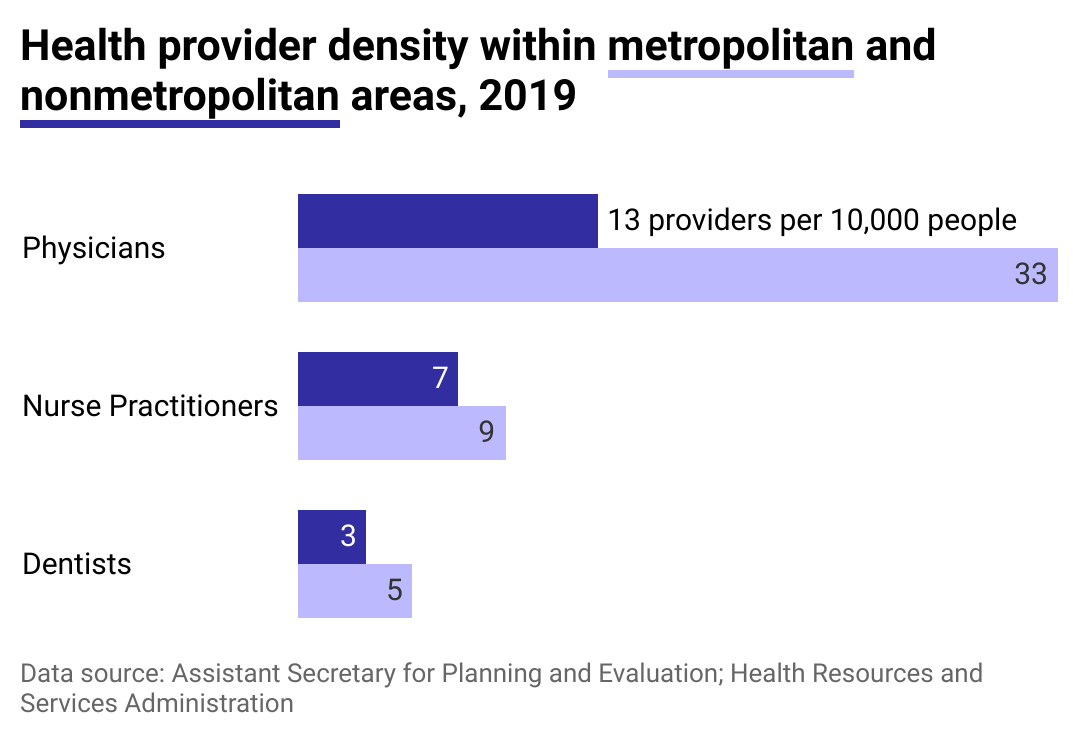
There are fewer health care providers per capita in nonmetropolitan areas
Although nearly 20% of the U.S. population lives in rural areas, . According to data from 2018 and 2019 that was released in 2021 by the, nonmetropolitan areas have fewer than half as many physicians per 10,000 people as metropolitan areas. Primary care providers and are in particularly short supply. For nursing shortages, the gap is slightly better, but there are still only seven nurse practitioners per 10,000 people in rural areas.

1 in 4 rural teens鈥攁nd 1 in 5 rural adults鈥攄on't have a primary care doctor who they see regularly
The lack of primary care physicians in rural populations is particularly troubling. Patients who regularly see a primary care physician tend to over their lifetimes. Additionally, many Americans consider a primary care doctor a trusted source of advice: A reported that rural adults said that their health care provider was the most trustworthy source of information about the COVID-19 vaccine. Four percent of unvaccinated adults said that the reason they weren't vaccinated is that they didn't have a primary care provider.
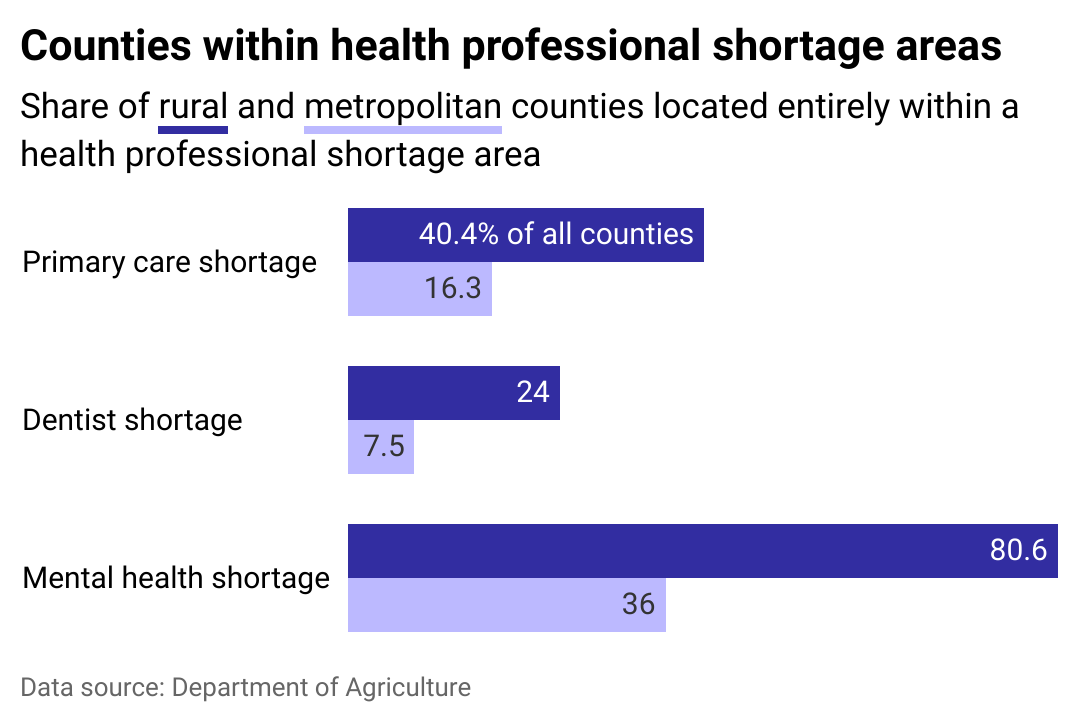
Compared to metropolitan areas, there are more than twice as many rural counties in health professional shortage areas
Data released in 2022 by the Department of Agriculture shows that rural counties are of primary care doctors, dentists, mental health care providers, and even hospitals.
Rural residents are also more likely to have to travel farther to access medical care. A found that rural residents drive 17 minutes on average to the nearest hospital鈥攎ore than five minutes longer than the average driving times for suburban and urban residents. An extra five minutes might not sound like much, but it can make a big difference in a medical emergency.

Medical practices in the most rural locations treat four times as many Medicare patients as metropolitan practices
When a community has only a few health care providers, those practices end up with a much heavier workload. Research released in 2022 found that more isolated practices with fewer physicians . Practices in urban and suburban settings typically offer 鈥攁n attractive proposition for new doctors.

142 rural hospitals have closed since 2010
Out of 185 rural hospitals that have closed since 2005, . A 2022 study found that contributed to most of these closures. Because rural hospitals typically treat more patients on Medicare and Medicaid, they often receive lower reimbursements than they would for patients with private insurance.
The patient mix in rural hospitals is also frequently older, poorer, and sicker than hospitals in urban or suburban settings. Making matters worse, when a rural hospital closes, it doesn't just make it more difficult for residents of that community to get medical care鈥攊t can also harm the local economy by cutting physician and nursing jobs, as well as dozens of related jobs in the community ranging from food services to cleaning and transportation.

1 in 5 medical schools ran a formal rural program in 2019
Attracting recent medical school graduates to rural areas is crucial to reducing the rural doctor shortage. However, although most medical schools offered some rural clinical experience, operated a formal rural program in 2019.
offer medical students hands-on experience in communities where a primary care doctor might be the only physician for miles, forcing them to expand their scope of practice to cover specialties like obstetrics. That expanded workload doesn't translate into additional stress: found that rural physicians in South Dakota experienced lower rates of burnout than their peers in cities or suburbs.

Hundreds of millions of dollars are going toward mitigation efforts and solutions for this shortage
Addressing the rural doctor shortage will likely require a combination of several different approaches. Building on the existing rural training programs, the Department of Health and Human Services announced to teaching health centers that focus on providing primary care and mental health care to underserved rural communities.
Creating pre-medical pipeline programs in rural communities can also help high school and college students see themselves entering medicine, which could bolster the rural applicant pool. The within the HRSA also runs several projects aimed at providing better access to telehealth services for rural communities.



