95% of women in menopause aren't offered treatment: Here’s how to get needed care
95% of women in menopause aren't offered treatment: Here’s how to get needed care
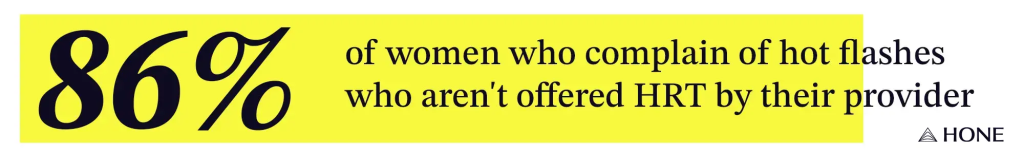
Hot flashes. Night sweats. Brain fog. For 85% of women, menopause symptoms derail sleep, work, and relationships. Yet are treated with hormone replacement therapy (HRT), the most effective way to relieve these symptoms.
This is despite showing HRT is safe for healthy women under 60 or within 10 years of menopause. The reasons? Doctors often aren’t trained to recognize or treat menopause, and many still cling to outdated fears, reports.
Doctors Don’t Learn About Menopause in Med School
A published in the journal “Menopause” revealed that just 30% of residency programs offer a dedicated menopause curriculum. In a , only 7% of OB-GYN residents felt “adequately prepared” to manage patients in menopause. About one-third said they wouldn’t offer to a symptomatic, newly menopausal woman, despite evidence that it could dramatically improve her quality of life.
This lack of training leaves women searching for answers in exam rooms where doctors aren’t equipped to treat them. Preliminary results from a —presented at the Menopause Society’s 2024 annual meeting—suggest that when women report symptoms like , , and , their doctor may not identify them as being associated with perimenopause or menopause.
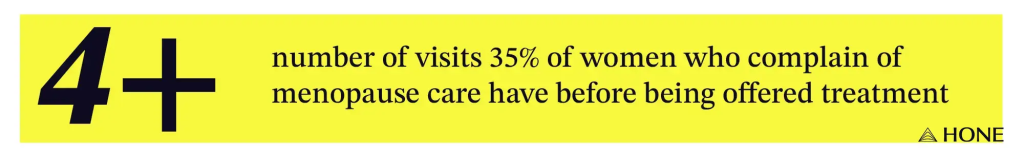
A ” in 2024 suggests that less than 14% of women with moderate or severe received any treatment in primary healthcare visits. Only 25% of women were identified by their providers as being in perimenopause or menopause during their first visit; 35% had to see their providers four or more times before their symptoms were linked to hormone changes.
A Leading Cause of Major Menopause Misinformation
The problem is compounded by fallout from the , a landmark study that seemed to suggest that hormone therapy significantly increased risks for breast cancer and heart disease.
The data was later reanalyzed and found to be misleading, but the damage was done. shows the share of U.S. women who were on dropped from a peak of around 42% in 2001 to 4.7% by 2017–2020, and it hasn’t rebounded.
“The way the findings were publicized by the media led to widespread fear around hormone therapy, both among patients and physicians,” says Tina Zhang, M.D., director of the Academic Women’s Health Fellowship in General Internal Medicine at Johns Hopkins.
Education on menopause was cut from residency programs, leaving younger doctors without mentors who knew how to confidently, says physician Heather Hirsch, M.D.
The Cost of Being Ignored
“In the short term, untreated menopause symptoms like , , , and can drastically reduce quality of life and affect , , and ,” says Zhang. “Long term, the menopausal transition is associated with , increased , and .”
It’s also going to affect how symptomatic your perimenopause and menopause experience will be, says Mache Seibel, M.D., a women’s health and menopause expert. “Your is going to be a lot shorter if you’re on ,” he says. “Your quality of life and the impact on your work life will be noticeably improved.”
How to Get Good Menopause Care Now
Women deserve informed, compassionate care in perimenopause and menopause. While physicians and educators continue to improve provider education, here are seven things every woman can do to get better menopause care right now.
- . Having a better understanding of menopause and related symptoms will help you communicate your concerns to your doctor and share knowledge with other women. “The more we normalize conversations around menopause, the more pressure we place on the healthcare system to catch up,” says Zhang.
- Get information from trusted sources like the Menopause Society, the National Menopause Foundation, the American College of Obstetricians and Gynecologists, and the International Menopause Society.
- Seek out providers who offer evidence-based menopause care. There are an increasing number of dedicated clinics for menopause and women’s midlife health in the U.S., says Zhang. The Menopause Society also offers certification in menopause care, so you can find a list of Menopause Society Certified Practitioners on their site. Otherwise, look for providers whose credentials include M.S.C.P., which stands for Menopause Society Certified Practitioner.
- Don’t settle. “If your provider is reluctant to engage in a conversation about menopause, it’s okay to find someone else,” says Zhang. “There are providers who want to help and who have the expertise to provide evidence-based guidance on how best to manage these symptoms.” You can also consider seeing a (in person or through telehealth) while still going to your main healthcare provider or gynecologist for primary care and routine exams.
- Prep for appointments. Keep a symptom log and a list of questions, and bring them to your appointment. Be sure to mention if you are experiencing , , sexual discomfort, , or any other symptoms (even if you’re not sure they’re related to menopause)—and ask about and treatment options that may help.
- Listen to your body and mind. “Perimenopause can present in a lot of different ways, so if something doesn’t feel right or you , it’s important to talk to your doctor,” says Seibel. “You don’t have to wait until you’re absolutely in menopause to be treated.”
- Reject the stigma. Don’t be afraid to talk about menopause or ask questions. Check in with your friends and find out what they’re doing to manage symptoms, suggests Seibel. It’s a significant change, but it’s one that all women transition through. And while it has its challenges, it’s not all negative. “Try to look at it as a life cycle transition into wisdom, maturity, and experience,” says Seibel. And remember, you’ll get through it.
Improving menopause education and patient care isn’t about prescribing one solution for all women—it’s about developing and providing science-backed, evidence-based guidance and treatment options, listening to women, and helping them understand which options might be most helpful to them.
was produced by and reviewed and distributed by Â鶹Դ´.