
A hydration guide for people on GLP-1s
Glucagon-like peptide 1 receptor agonists (GLP-1 RAs) are used to treat obesity, Type 2 diabetes, and more. These medications, while helpful for these conditions, could indirectly cause fluid or electrolyte imbalances. shares what to watch for and how to strategize with electrolytes.
Glucagon-like peptide-1 receptor agonist (GLP-1 RA) medications ā sold under the blockbuster brand names Ozempic, Wegovy, Mounjaro, and more ā have dominated headlines in recent years.
These marvels of modern medicine help treat the chronic conditions of obesity and Type 2 diabetes. They do this by mimicking the natural GLP-1 gut hormone, which has beneficial effects on glucose (blood sugar), appetite management, and more.
Theyāve revolutionized weight management and diabetes care, and these effects are much talked about on social media and beyond.
Whatās rarely discussed is how these medications may affect your bodyās electrolyte levels ā something people taking them should be aware of.
More research is needed on how GLP-1 RAs affect electrolyte balance (and itās likely highly individual depending on each personās unique circumstances), but the topic deserves attention given hydrationās role in metabolic health.
This article explores how GLP-1 RAs work, why they might alter your and electrolyte needs, how lifestyle changes play a role, strategies for maintaining proper fluid and electrolyte balance, and red flags to watch for.
What Are GLP-1s and Why Are Electrolytes Important?
āGLP-1 is a keystone hormone of metabolism with a wide range of metabolic effects,ā says , a leading voice in the science of metabolic health.
GLP-1 RAs mimic the bodyās natural GLP-1 gut hormone, which people who have or may secrete less of.
When it comes to weight management and Type 2 diabetes, GLP-1 RAs:
- Help with blood sugar regulation and improve .
- Alter the the brain receives.
- , the rate of food moving from the stomach to the small intestine.
āGLP-1 RAs are dosed in such a way as to give supraphysiologic levels of the hormone,ā Dr. Norwitz says.
āTherefore, at a high level, itās easy to see why ā and electrolyte balance ā could be altered by starting GLP-1 RA therapy.ā
In other words, these medications deliver higher hormone levels than your body produces naturally. Because they influence how your body processes energy and manages key functions, they can also affect electrolyte balance.
Why GLP-1 users need to pay attention to electrolytes
Because of the effects GLP-1 RAs have on digestion and appetite signals, GLP-1 users may eat less, drink less, and absorb less, explains , department head of critical care at The Ottawa Hospital.
āTogether, this increases the risk of dehydration and electrolyte imbalances ā even in people who donāt feel sick,ā he adds.
Some people might also experience medication side effects, such as which could contribute to further alterations in hydration and electrolyte balance.
Why does electrolyte balance matter in the first place? The body requires to maintain fluid balance and aid with muscle, nerve, and brain function, along with various other bodily processes. These are:
- Sodium
- Potassium
- Calcium
- Magnesium
- Chloride
- Phosphate
- Bicarbonate
āIf youāre not eating or drinking enough, especially while losing weight rapidly, you may be quietly developing deficiencies even if youāre taking your medication exactly as prescribed,ā Dr. Kyeremanteng says.
But managing your fluid and electrolyte balance while taking a GLP-1 RA is not a one-size-fits-all approach.
āThe specific mechanisms by which GLP-1 RAs could impact electrolyte balance will differ depending on the individual and may include ādirect effects,ā such as altering insulin levels and influencing sodium handling by the kidneys, or āindirect effects,ā such as decreased food, fluid, and electrolyte intake, or gastrointestinal side effects like nausea and vomiting,ā Dr. Norwitz says.
Bottom line: GLP-1 RAs can affect your electrolyte balance through multiple pathways ā both directly (by changing how your body processes sodium and insulin) and indirectly (by reducing your food and fluid intake or causing GI side effects). Because everyoneās response is different, itās important to pay attention to your hydration and electrolyte needs while taking these medications, even if youāre not experiencing obvious symptoms.
How Key Electrolytes Are Affected by GLP-1 Use
Researchers havenāt investigated the exact effects a GLP-1 RA medication might have on electrolytes, let alone the different versions.
āThere is no hard-and-fast rule that taking a GLP-1 RA will do āXā to āYā electrolyte,ā Dr. Norwitz says, ābut itās worth being mindful that shifts are possible. People who experience persistent vomiting or who have kidney disease may be at higher risk for electrolyte disturbances.ā
Keep in mind that electrolytes often work in concert with each other. For example, we have a protein on all our cell membranes called the , and as the name implies, it requires both electrolytes (sodium and potassium) in specific quantities to facilitate nerve signaling and muscle contraction.
So instead of focusing on how GLP-1 RAs might affect each individual electrolyte, a more helpful approach is to understand what complications might arise from GLP-1 usage and when they warrant attention.
"It depends on how an individual responds to their GLP-1 RA," Dr. Norwitz says.
The most common electrolyte-related issues stem from two primary mechanisms:
- Gastrointestinal losses (from vomiting or diarrhea)
- Reduced dietary intake (from appetite suppression)
Hereās what can happen and what matters.
Metabolic alkalosis (persistent or severe vomiting)
"Repeated vomiting can lead to a loss of chloride and potassium, often with (an increase in blood pH) and altered sodium levels," Dr. Norwitz says.
When to be concerned: If youāre vomiting frequently (multiple times per day or for more than 24 hours), especially if accompanied by severe muscle cramping or unusual irritability, contact your doctor.
Occasional nausea is common with GLP-1 RAs, but persistent vomiting (GLP-1 related or not) can deplete electrolytes significantly.
Hyponatremia and hypernatremia (sodium imbalance)
Sodium abnormalities typically only occur when significant vomiting, diarrhea, dehydration, or excessive water intake accompany GLP-1 RA use.
"Sodium can trend low () if large amounts of free water are consumed without adequate electrolytes, or high () if fluid intake is inadequate," Dr. Norwitz says.
People are most at risk if they eat very little food while drinking too much plain water, or if they become very dehydrated.
When to be concerned: Sodium imbalances become serious when they cause confusion, severe weakness, or (in extreme cases) seizures. Mild like occasional headaches or fatigue are common with GLP-1 RAs and donāt necessarily indicate a sodium problem, but if you experience confusion or severe muscle weakness, get evaluated.
Hypomagnesemia and Hypocalcemia (severely reduced food intake)
"People taking GLP-1 RAs may experience a decrease in magnesium and calcium intake as a result of reduced overall dietary intake," Dr. Norwitz adds.
When to be concerned: Low magnesium () and low calcium () typically develop gradually. Severe deficiencies can cause persistent muscle cramping, unusual tingling, or confusion but these symptoms usually appear only after a prolonged time of eating very small amounts.
Bottom line: If youāre eating very little for extended periods, consider having your doctor check your electrolyte levels proactively rather than waiting for symptoms.
Recognizing Signs of Dehydration and Electrolyte Imbalances ā and What to Do
āThe most common electrolyte shifts with GLP-1 RA use, when they occur, are losses of chloride and potassium from vomiting, sometimes accompanied by changes in sodium levels,ā Dr. Norwitz says.
āBecause sodium can go either low or high, depending on hydration and fluid replacement, symptoms can vary.ā
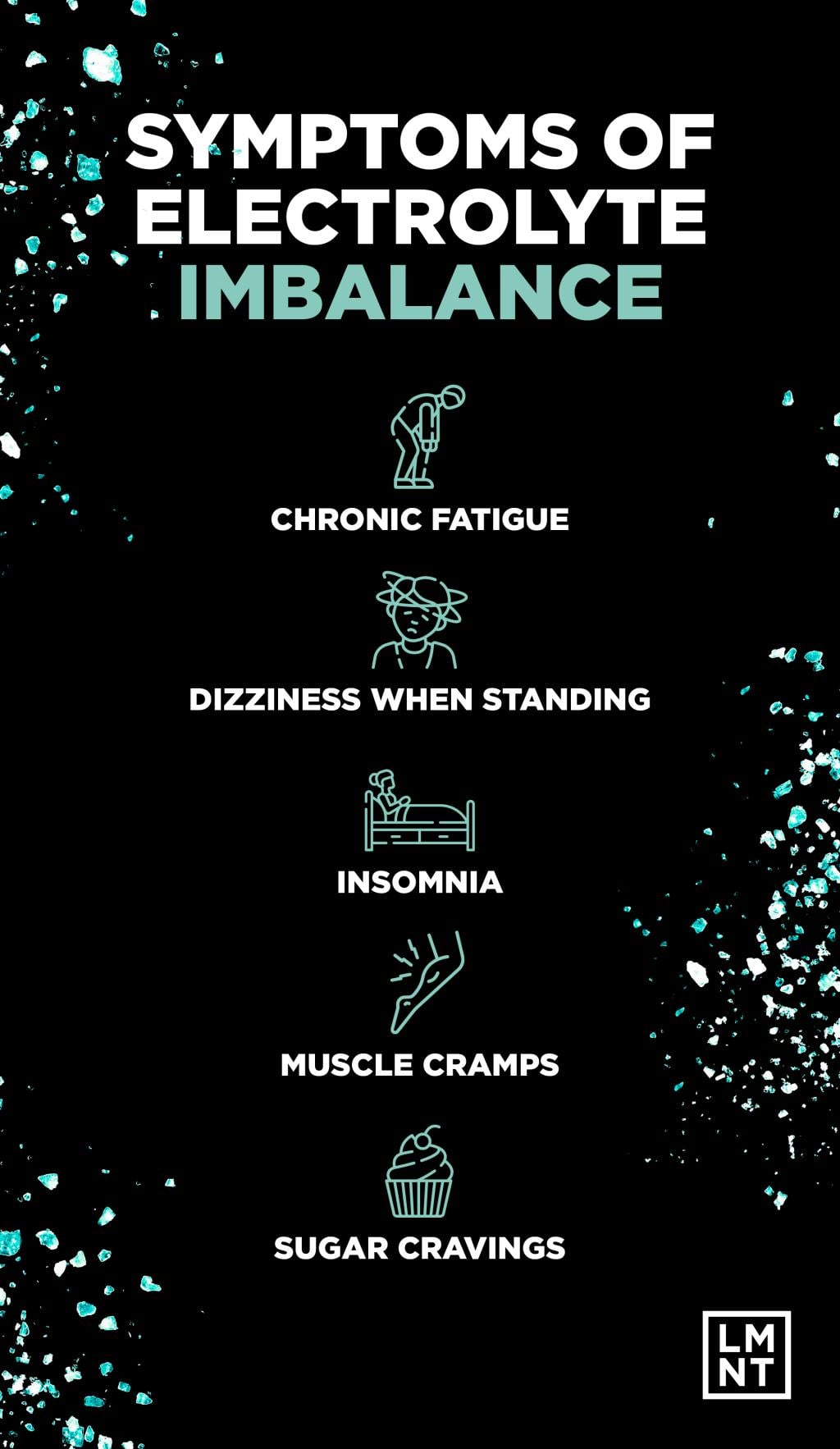
include:
- Dark urine or urinating infrequently
- Dry mouth and lips
- Dizziness when standing
- Rapid heartbeat
- Extreme thirst
āThese symptoms are non-specific, meaning they can arise from many causes,ā Dr. Norwitz explains. āBut if they occur soon after starting a GLP-1 RA ā especially alongside vomiting, diarrhea, or poor oral intake ā electrolyte imbalance should be on the list of possibilities.
What to do: If you notice signs of dehydration, increase fluid intake with electrolyte-containing beverages rather than plain water alone. Plain water without electrolytes can dilute sodium levels further, potentially worsening the problem.
If dehydration is severe (little to no urination, extreme weakness, confusion), seek medical attention. Further action may be necessary.
A Practical Approach to Monitoring
Many symptoms of electrolyte imbalance ā fatigue, occasional muscle cramps, mild nausea ā are also common side effects of GLP-1 RAs themselves and donāt necessarily signal a problem.
Focus on these red flags:
- Persistent vomiting (more than 24 hours)
- Severe or worsening muscle weakness
- Confusion or significant mental changes
- Seizures or loss of consciousness
Consider proactive testing if you:
- Experience frequent vomiting or diarrhea
- Have drastically reduced food/fluid intake for weeks
- Take diuretics or have kidney conditions
- Feel unusually unwell beyond typical medication adjustment
When in doubt, a blood panel can measure your electrolyte levels and provide clarity. You donāt need to self-diagnose which specific electrolyte is off. Your doctor can help determine that and advise accordingly.
Benefits of Electrolytes for GLP-1 users
āGLP-1s are helping people transform their metabolic health,ā Dr. Kyeremanteng says, ābut that transformation needs to be supported. Hydration and electrolyte balance arenāt just ānice-to-haves.ā Theyāre part of how you keep intact during and metabolic reset.ā
A key thing to remember is that electrolytes are essential, and GLP-1 RAs and other factors may alter your needs. GLP-1 RA medications work best in conjunction with , which may include changes to your diet and exercise plans.
Even when people have already been engaging in healthy habits prior to taking a GLP-1 RA, they may find that the medication helps build further momentum and motivation to make lifestyle modifications.
But these changes may bring about the need for increasing your electrolyte intake, to avoid fatigue, reduced exercise , brain fog, or other symptoms. Hereās more info on how lifestyle changes may boost your electrolyte needs.
Diet
As you start a GLP-1 RA, reduced appetite may lead you to , while reduced cravings may change what you choose to eat.
Since GLP-1 RAs have only recently become more ubiquitously used, researchers are still trying to understand how they affect eating habits.
Survey results suggest that GLP-1 RA users are eating more fruits and vegetables, , and even eating fewer carbohydrates.
These shifts reduce sodium intake for a few reasons:
- The average American gets the bulk of their sodium from . When you eliminate or drastically reduce these products, youāre also eliminating your primary sodium source. Whole foods like fruits, vegetables, and unprocessed proteins contain very little sodium naturally. For example, a chicken breast has about 70mg of sodium, while a bag of chips has 1,500mg. When you shift to a predominantly whole-foods diet, youāre not just reducing sodium ā youāre removing nearly all of it. Unless youāre actively adding salt to your food, youāre likely consuming far less sodium than your body needs.
- People on low-carbohydrate diets in urine, further increasing sodium requirements.
So if youāre eating mostly whole foods on a GLP-1 RA, youāll likely need to intentionally add sodium to meet your bodyās needs.
Exercise
If youāve increased your , you will lose more sodium, chloride, and potassium through sweat.
Compounding the issue is that more intense or longer exercise sessions can also cause you to lose even more of these electrolytes, especially if performed at higher temperatures.

How to safely incorporate electrolytes into your routine
If youāre taking a GLP-1, you may be wondering how to keep your electrolytes balanced.
āBecause the electrolyte effects of GLP-1 RAs are highly individual and often depend on side effects such as nausea, vomiting, or dramatically reduced food intake, broad generalization would be overreaching,ā Dr. Norwitz says.ā
āHowever, if someone experiences symptoms like fatigue, dizziness, muscle cramps, or persistent vomiting ā especially in the context of dietary changes that lower electrolyte intake ā they should consider targeted electrolyte replacement,ā he adds.
āThat might mean using rehydrating with an electrolyte-containing beverage that provides sodium, potassium, and chloride, rather than only drinking plain water, until symptoms resolve.ā
Salt is made up of sodium chloride, so it provides two electrolytes.
āThe goal is to address both fluid and electrolyte needs. As is the case in vomiting, restoring only fluid (i.e., plain water) can lead to low sodium levels and worsen symptoms,ā Norowitz concludes.
Dr. Kyeremanteng also notes that GLP-1s can blunt appetite, so you canāt rely on food alone to meet your electrolyte needs.
āElectrolyte supplementation becomes a smart strategy, not a bonus. Your thirst signal may be reduced on GLP-1s. Make hydration and electrolyte intake a part of your daily routine, not just something you respond to.ā
If youāre adding electrolytes as part of your regular routine to support overall fluid balance and exercise performance, here are a few considerations:
- Determine your sodium needs. A considers diet, activity level, climate, and more. This type of tool can help you build strategies around your electrolyte use ā but keep in mind it doesnāt take GLP-1 RA symptoms like diarrhea or vomiting into account. Those side effects increase your electrolyte needs.
- Experiment with electrolytes strategically throughout your day: Consider adding electrolytes in the morning (especially if you skip breakfast), during or after exercise (depending on duration), if youāre spending time in a warm environment and sweating, and on days with low food intake or if youāre experiencing any gastrointestinal side effects, Dr. Kyeremanteng says.
- Donāt forget dietary sources: āBe mindful to consume adequate and calcium ā either from dietary sources (potassium: avocado, salmon, beets, zucchini; calcium: low-sugar yogurt, kefir, cheeses; magnesium: dark chocolate, pumpkin seeds) or through supplementation if needed.ā

Key takeaways
- GLP-1 RAs are useful tools for weight and diabetes management, but they may indirectly alter your electrolyte needs.
- Medication side effects, reduced appetite, lifestyle changes, and more can all contribute to electrolyte imbalances.
- But you can create strategies around adding electrolytes to your routine to help maintain fluid and electrolyte balance and to support your lifestyle changes.
- If you develop medication side effects or symptoms of an electrolyte imbalance, talk to your prescribing healthcare provider.
FAQ
Do electrolytes directly help with weight loss?
Electrolytes donāt directly help with weight loss, but theyāre necessary for normal metabolic function, including and
One caveat: Some electrolytes contain added sugar, and this addition can counteract weight management efforts or worsen prediabetes or Type 2 diabetes.
Do I need electrolytes on a GLP-1?
GLP-1 medications, used to treat obesity and Type 2 diabetes, can cause side effects, such as vomiting or reduced appetite (leading to less food consumption), which could change your electrolyte needs. Whether you need electrolyte supplementation while taking these medications will depend on your unique circumstances. Talking to the healthcare provider who prescribed your medication can help you determine if you need supplementation.
Can GLP-1 cause low potassium?
Taking a GLP-1 may lead to low potassium if you are eating fewer because of a reduced appetite, exercising more (and therefore sweating more), or if youāre experiencing medication side effects, such as vomiting or diarrhea.
was produced by and reviewed and distributed by Ā鶹Ō““.



