
Why aging causes flu-like body aches in women
Why aging causes flu-like body aches in women
You wake up feeling like youāve run a marathon, even though you didnāt work out. Your body feels heavy, sore, and achyāalmost like youāre coming down with something. But youāre not sick. Whatās happening?
More than of women in midlife experience body aches, whole-body muscle soreness, muscle fatigue, stiff or swollen joints, aching bones, and other pain symptoms.
āThese kinds of discomforts are a very real and often frustrating part of the journey that can come on gradually and insidiously,ā explains Natalie Kunsman, M.D., a family medicine physician who treats women in this age group.
Many chalk it up to old age or arthritis, but hormones are often to blame, reports.
If youāre in your 40s and have never felt these sensations before, plus youāre having ā, , , , , , and āthen signs point to hormonal fluctuations.
How Hormones Drive Body Aches
As estrogen and progesterone decline in midlife, the bodyās balance shifts in ways that can make you more sensitive to pain.
Estrogen keeps muscles and bones strong, lubricates joints, and . When levels drop, it can lead to increased stiffness, muscle soreness, and joint pain, explains womenās health expert and OB-GYN Kecia Gaither, M.D.
on the nervous system and helps dial down pain. When it declines, pain receptors become more active.
Together, low estrogen and progesterone prime the body for pain.
Orthopedic surgeon and aging specialist Vonda Wright, M.D, first coined the term āmusculoskeletal syndrome of menopauseā in a to describe the constellation of muscle, joint, and bone pain that comes with declining estrogen levels during the menopausal transition. Her research was the first to validate the experiences of many women who report feeling like their bodies are āfalling apartā despite no obvious injury.
The PaināInflammation Loop
Lower estrogen doesnāt just stiffen jointsāit can also affect the immune system, ramping up āWhen estrogen levels start to fluctuate, it can raise histamine levels [which stimulates inflammation] and disrupt the regulation of anti-inflammatory cytokines (signaling proteins), leading to muscle and joint stiffness,ā Kunsman says.
Add in muscle loss from declining estrogen and reduced activity, and the pain cycle can intensify. Weaker muscles provide less support for joints, leading to instability and discomfort.
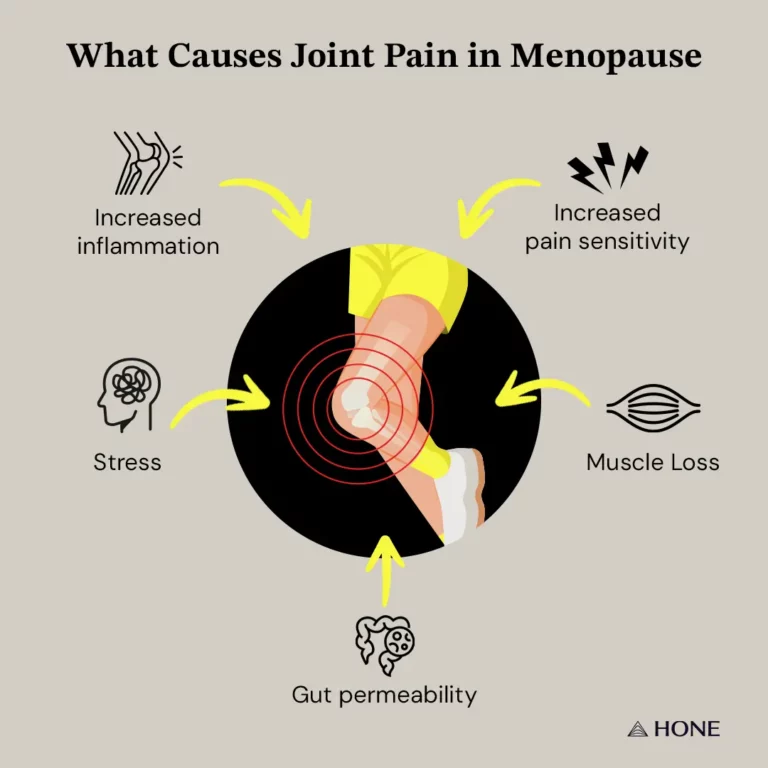
Some women also notice heightened pain sensitivity. āHormones, especially estrogen, modulate pain signals,ā Kunsman says. āWhen estrogen drops, pain perception may increase.ā This may explain why chronic pain conditions such as fibromyalgia often first appear or worsen during the transition to menopause.
Fluctuating estrogen levels can also disrupt gut bacteria that help regulate hormones, triggering inflammation and contributing to bloating, fatigue, and body-wide aches.
Chronic stress compounds the problem by raising cortisol and lowering recovery hormones, creating a vicious cycle where stress and pain feed each other.
Lifestyle fixes that help
Before turning to medication, both doctors recommend addressing the root cause through movement, nutrition, and stress management.
Move more
Staying active protects against muscle loss and helps control inflammation. preserves lean muscle mass, while moderate aerobic activity lowers pro-inflammatory markers. also releases endorphinsāthe bodyās natural painkillers. āIf youāre starting new workouts, make sure to stretch and recover between sessions,ā says Kunsman.
Adjust your diet
A of proven , including avocados, berries, broccoli, dark chocolate, , mushrooms, and olive oil can help calm inflammation.
Minimize processed foods, refined sugars, and alcohol. Gaither suggests adding foods with phytoestrogens (like soy and flaxseed) to mimic estrogenās positive effects, and plenty of calcium and vitamin D to protect bones.
Support your gut
Hormone shifts also alter gut bacteria, which can increase inflammation and pain. āSupporting gut health with probiotics and fiber helps restore balance,ā says Gaither.
Manage stress
Feeling calm and in control helps keep cortisol in check, which helps prevent and ease stress-induced inflammation and body aches. Try yoga, walking, deep breathing or meditation and mindfulness. These improve mood-enhancing hormones and activate the , which helps your body relax.
When to Consider Hormone Therapy
Hormone replacement therapy (HRT), also commonly called (MHT), typically involves estrogen or a . In some cases, is added to improve muscle mass, libido, , , and bone density.
MHT is to help relieve debilitating menopause symptoms, including hot flashes, , and joint pain. A study in the journal also found that women who took suffered less joint pain even though they had more joint swelling.
was produced by and reviewed and distributed by Ā鶹Ō““.



